Sharing scientific news-related content on global infectious diseases.
  
|
Posted By By ISID Emerging Leader, Dr. Massab Umair,
Tuesday, April 15, 2025
|
During the height of the COVID-19 pandemic, I had the rare privilege of presenting genomic surveillance data and other laboratory insights at Pakistan’s National Command and Operation Center (NCOC). It was more than just a professional milestone—it was a front-row seat to one of the most remarkable crisis management operations in the country's history. The NCOC wasn’t just a command center; it was a game-changer, transforming fragmented efforts into a unified national strategy. Pakistan’s ability to tackle the pandemic—and now the Mpox threat—didn’t happen by chance. It was the result of a centralized, data-driven approach that many still don’t fully appreciate.
When COVID-19 first hit Pakistan in early 2020, the nation stood at a crossroads. With a fragmented healthcare system and governance challenges stemming from the 18th Amendment, which devolved health responsibilities to the provinces, a coordinated response seemed nearly impossible. Yet, against all odds, Pakistan emerged as one of the few countries that managed to navigate the crisis with remarkable efficiency. The secret weapon? The National Command and Operation Center.
As the nerve center of Pakistan’s pandemic response, the NCOC became a beacon of centralized decision-making and data-driven governance. It transformed what could have been a chaotic, disjointed effort into a streamlined and effective national strategy. And now, as Pakistan grapples with a looming threat in the form of Mpox (formerly monkeypox), the NCOC’s legacy continues to shape the country's response.
A Blueprint for Crisis Management
When COVID-19 struck, developed nations with robust healthcare infrastructures faltered. Pakistan, despite its resource limitations, took a different approach: it established a unified command. Using constitutional provisions to bypass bureaucratic bottlenecks, the federal government created the NCOC in April 2020. This body did what few expected—it brought all provinces, health agencies, and security forces onto the same page.
Led by the Minister of Planning and Development, with military leadership providing operational expertise, the NCOC crafted policies that balanced public health and economic stability. Unlike blanket lockdowns that paralyzed many economies worldwide, Pakistan introduced smart lockdowns—a targeted strategy that restricted only high-risk areas. This approach not only curbed the virus’s spread but also kept businesses afloat, mitigating economic devastation.
The NCOC’s achievements were staggering. COVID-19 testing capacity skyrocketed from just four laboratories to over 170 nationwide. Daily testing rose from 500 to an impressive 65,000. The “Test, Trace, and Quarantine” strategy helped contain outbreaks, while aggressive vaccination campaigns, backed by real-time data analysis, ensured effective immunization coverage. One of the hallmarks of the NCOC during the COVID-19 pandemic was its ability to make quick
decisions. I remember advocating for genomic surveillance and the need to strengthen next- generation sequencing (NGS) facilities at NIH. Given the high costs of NGS technology, securing funding seemed unlikely. However, to my surprise, the proposal was swiftly approved by the Special Assistant to the Prime Minister (SAPM) on Health—who, being an infectious disease expert, recognized its critical importance. With these funds, NIH was able to report variants and their spread in real time to the NCOC, significantly aiding data-driven decision-making. Additionally, the NCOC played a key role in shaping public behavior through strategic communication. Initially, many citizens underestimated COVID-19’s severity, but by mid-2020, the NCOC’s multi-platform messaging—through media campaigns and mobile phone alerts— helped drive compliance with mask-wearing and social distancing. By the time the NCOC wound down operations in April 2022, it had successfully steered Pakistan through six waves of the pandemic.
NCOC 2.0: Taking on Mpox
While many saw the NCOC’s closure as the end of an era, its operational framework proved too valuable to retire completely. In 2024, as Mpox cases surfaced worldwide, Pakistan was quick to react. The NCOC was reactivated (this time led by National Institute of Health (NIH), leveraging its pandemic-tested model to preempt a full-blown crisis.
Despite initial WHO recommendations against screening travelers at entry points, Pakistan took a proactive stance. Border Health Services, under NCOC directives, implemented early screenings, leading to the timely detection of imported Mpox cases. Public health laboratories across the country, in collaboration with the NIH, ramped up diagnostic capacities, while the polio environmental surveillance network was repurposed to track Mpox outbreaks. These measures allowed Pakistan to detect and contain 14 cases as of March 2025—before the virus could spiral into an uncontrollable epidemic.
Genomic surveillance, another NCOC hallmark, has played a crucial role in tracking Mpox mutations. Scientists at NIH have successfully sequenced and identified imported viral strains, helping public health officials anticipate transmission patterns. Meanwhile, isolation protocols and containment strategies, similar to those deployed during COVID-19, are ensuring that Pakistan stays ahead of the curve.
Lessons for the World
Pakistan’s handling of COVID-19 and now Mpox underscores an invaluable lesson: centralized coordination works. The NCOC model—grounded in data, rapid decision-making, and inter- agency collaboration—has proven that even countries with limited resources can effectively manage global health crises.
While international recognition has poured in, with WHO commending Pakistan’s pandemic response, the real victory lies in the blueprint it offers for future public health emergencies. Whether it’s a resurgence of COVID-19, another viral outbreak, or an unforeseen health crisis, Pakistan now possesses a tested and scalable mechanism to respond.
As global health threats continue to evolve, perhaps it’s time for other nations to take a page from Pakistan’s playbook. The NCOC didn’t just help Pakistan survive a pandemic—it set a precedent for how nations can turn adversity into opportunity through strategic, science-backed governance.
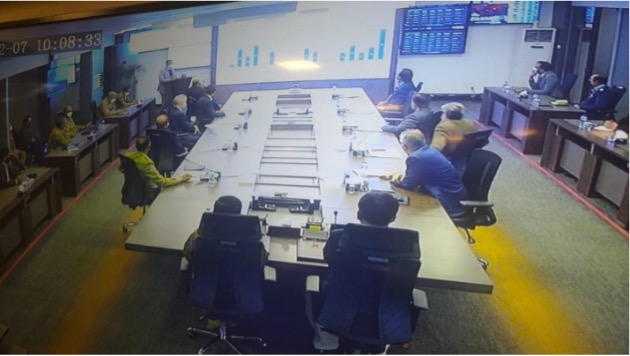
Dr. Massab Umair Presenting Genomic Surveillance Data on SARS-CoV-2 at NCOC: Informing Pakistan’s Pandemic Response.
By ISID Emerging Leader, Dr. Massab Umair
The author is a virologist and public health expert with a focus on disease surveillance and health systems strengthening (massab.umair@yahoo.com).
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By ISID Emerging Leader, Dr. Nadia Noreen,
Friday, April 4, 2025
|
Every year, World Health Day provides a timely opportunity for nations to reflect on the progress in advancing health equity and renew their commitment to building resilient and inclusive health systems. In 2025, as the global community intensifies its efforts toward universal health coverage (UHC), Pakistan stands at the forefront, reaffirming its dedication to strengthening primary health care (PHC) and embracing digital transformation to meet the evolving needs of its population.
Embracing Digital Transformation in Health
Pakistan has taken bold strides toward digitalizing its health infrastructure, recognizing technology's transformative potential in improving service delivery, continuity of care, and patient safety. Furthering these efforts, the country piloted Electronic Medical Records (EMR) and a one-patient-one-ID system in the Islamabad Capital Territory (ICT), setting a foundation for nationwide integration.
Looking ahead, Pakistan envisions a digitally integrated healthcare system that includes the nationwide rollout of Electronic Medical Records (EMR) to digitize health records and streamline information management. Implementing a "One Patient, One ID" model is expected to enhance care continuity and reduce fragmentation across various health system levels. Also, establishing hospital bed registries and structured referral systems will improve coordination between primary and tertiary care facilities. Ensuring the availability of essential diagnostics and medicines at the point of care remains a top priority to enhance service delivery and meet patients' needs efficiently.
Reinventing Primary Health Care
Pakistan firmly believes that primary health care is the cornerstone of UHC. Strengthening PHC supports routine services and acts as a first line of defense in maternal and child health, disease surveillance, and emergency preparedness. To realize this vision, Pakistan has developed a contextualized Essential Package of Health Services (EPHS) that is being rolled out at the community level, primarily through its vast Lady Health Workers (LHWs) Program. Lady Health Workers Program: is a Community-Based Backbone launched in 1994; the LHWP has grown into one of the most extensive community-based health programs in the world. With approximately 90,000 LHWs, they deliver services to around 115 million women and children, serving as key links between communities and health systems, providing Family planning and contraceptive use education, Antenatal, natal, and postnatal care. Nutrition and hygiene promotion, Immunization support (including polio, malaria, TB, and routine under-five immunization), Disease prevention, and public health awareness.
To support their role in delivering EPHS, the LHW curriculum has been revised to align with UHC goals, and regular training modules are implemented to ensure updated knowledge and practices. Counseling cards cover 22 family care practices from conception to 8 years of age, emphasizing men's involvement in child development and care.
Tackling the Nutrition Crisis
Nutrition remains a significant public health challenge in Pakistan. An estimated 3% of GDP is lost annually due to malnutrition. Nearly half of Pakistan's children and mothers suffer from undernutrition, impeding human development and progress toward the Sustainable Development Goals (SDGs).
Pakistan has initiated a comprehensive package of nutrition interventions:
- Multiple Micronutrient Supplementation (MMS) integrated into antenatal care
- Fortification of staple foods
- Wheat flour with iron and folic acid
- Edible oils with vitamins A and D
- Vitamin A supplementation campaigns for children aged 6–59 months
- Promotion of Infant and Young Child Feeding (IYCF) practices
- Community-Based Management of Acute Malnutrition (CMAM)
- Strengthening nutrition data through integration into the District Health Information System (DHIS)
Strengthening Governance and Policy Frameworks
Digital transformation and efforts to achieve Universal Health Coverage (UHC) require strong policies and safeguards to ensure long-term success and equity. In this regard, Pakistan is actively working toward establishing comprehensive national and provincial digital health policies that foster innovation and uphold essential principles such as data privacy, ethical standards, and the protection of health workers' rights. These policies aim to guarantee equitable access to health services across all segments of society, including marginalized and vulnerable populations. Simultaneously, the government is focusing on coordinating health investments across federal and provincial levels, expanding healthcare coverage to underserved and remote areas, and building resilient health infrastructure capable of effectively responding to emergencies and outbreaks.
The Path Forward: A Collective Commitment
On World Health Day 2025, Pakistan reaffirms its commitment to building a future where health systems are proactive, prepared, and centered around the needs of people. The country envisions a healthcare landscape where technology is a powerful enabler, empowering healthcare providers and recipients to deliver and access more efficient, informed, and equitable care. Strengthening primary health care remains at the core of this vision, serving as the frontline defense against disease, health disparities, and public health threats. Pakistan is determined to ensure that every citizen—regardless of geography, income, or background—has access to safe, high-quality, and affordable healthcare, leaving no one behind in pursuing health and well-being.
Our Commitment to Health and Equity
Let us move forward with a shared resolve to #Empower communities #Embrace innovation #Strengthen health systems #Protect every health worker and citizen.
Stay healthy. Stay empowered. Let's build a digitally advanced, community-centered, and healthier Pakistan together.
Acknowledgement: Author would like to acknowledge the support received from Director General Health.
By ISID Emerging Leader, Dr. Nadia Noreen
Author is a medical graduate, Public Health specialist, and Epidemiologist with focus on international health regulations, global health security disease surveillance, and health systems strengthening.
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By ISID Emerging Leaders, Benjamin Kadia and Tintu Varghese,
Wednesday, March 26, 2025
Updated: Friday, April 4, 2025
|
The longstanding global crisis of childhood undernutrition
For years, global efforts to reduce childhood undernutrition have focused on the idea that “what you are is what you eat.” This approach has led to initiatives like promoting exclusive breastfeeding and improving sanitation and hygiene, backed by organizations like the World Health Organization (WHO). However, despite these efforts, the rates of childhood undernutrition worldwide have not dropped as expected[1]. This shows that we need new, innovative ways to strengthen existing programs and better support children’s health.
One major reason why childhood undernutrition remains a problem is due to enteric infections—infections that affect the intestines. Diarrhoea is one of the most common consequences of enteric infections, and it often leads to a cycle where children lose nutrients, feel less hungry, and cannot absorb nutrients properly, resulting in malnutrition[2]. In areas with poor sanitation and hygiene, children are also exposed to harmful microbes, which can cause a condition called environmental enteric dysfunction. This condition, which can be acquired as early as 12 weeks of age, damages the intestines, making it harder for children to digest and absorb nutrients[3].
Gut Health: The key to prevention
To prevent both enteric infections and undernutrition, we need to keep the intestines healthy. Interestingly, scientists are now looking at how probiotics (beneficial bacteria) and prebiotics (compounds that feed beneficial bacteria) can play a role in improving gut health and preventing infections. Probiotics are live microorganisms, often bacteria, that, when consumed in adequate amounts, can have a positive effect on health. Prebiotics, usually types of fibre, act as food for these good bacteria. Synbiotics combine both probiotics and prebiotics to support gut health.
In high-income countries, probiotics have been used for years to treat and prevent various childhood conditions, like diarrhoea and premature birth complications[4]. These beneficial bacteria work by improving the gut microbiota—the community of microbes living in our intestines. When we consume probiotics, they help increase the number of good bacteria, which compete with harmful pathogens for space in the gut. They also help digest food and produce acids that fight off bad bacteria, boost the growth of healthy intestinal cells, and support the immune system.
The future of gut health in fighting undernutrition
Most research so far on probiotics has focused on children who are already sick or older children. However, there is a growing interest in using probiotics from early childhood to help build a stronger, healthier gut from the start. Early studies, particularly in sub-Saharan Africa, are exploring whether giving probiotics to infants can improve their growth, development, and overall health. These studies suggest that the health of our intestines is just as important as the food we eat when it comes to fighting undernutrition[5].
In short, for children to fully process and utilize the nutrients in the food they eat, their intestines must always be strong and healthy. By improving gut health through probiotics, we could help children grow stronger, fight infections more effectively, and ultimately reduce the rates of childhood undernutrition.
By ISID Emerging Leaders, Benjamin Kadia and Tintu Varghese
References
- Scott N, Delport D, Hainsworth S, Pearson R, Morgan C, Huang S, et al. Ending malnutrition in all its forms requires scaling up proven nutrition interventions and much more: a 129-country analysis. BMC Med. 2020;18(1):356.
- Rodriguez L, Cervantes E, Ortiz R. Malnutrition and gastrointestinal and respiratory infections in children: a public health problem. Int J Environ Res Public Health. 2011;8(4):1174-205.
- Naylor C, Lu M, Haque R, Mondal D, Buonomo E, Nayak U, et al. Environmental Enteropathy, Oral Vaccine Failure and Growth Faltering in Infants in Bangladesh. EBioMedicine. 2015;2(11):1759-66.
- Alcon-Giner C. Microbiota Supplementation with Bifidobacterium and Lactobacillus Modifies the Preterm Infant Gut Microbiota and Metabolome: An Observational Study. Cell Reports Medicine 2020.
- Momo Kadia B, Otiti MI, Ramsteijn AS, Sow D, Faye B, Heffernan C, et al. Modulating the early-life gut microbiota using pro-, pre-, and synbiotics to improve gut health, child development, and growth. Nutr Rev. 2023.
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By ISID Emerging Leader, Massab Umair,
Wednesday, March 5, 2025
|
For decades, Pakistan has been engaged in an uphill battle against polio, a disease that was once on the brink of eradication. Yet, just when the country seemed close to victory, the virus has resurged with alarming intensity. In 2024, 74 cases of wild poliovirus type 1 (WPV1) were reported across 34 districts—a stark reminder that this crippling disease is far from being consigned to history.
The most severely affected region has been Balochistan, where 27 cases surfaced from 13 districts, with Killa Abdullah emerging as a new hotspot. Sindh recorded 23 cases, while Khyber Pakhtunkhwa (KP) documented 22, including 11 in Dera Ismail Khan (DI Khan) alone. Even Punjab and Islamabad were not spared, each reporting one case. The resurgence has been particularly troubling in DI Khan, which had remained polio-free since 2019.
A Setback for Pakistan’s Eradication Efforts
This surge in cases represents a significant setback for Pakistan’s polio eradication efforts. In contrast, in 2023, WPV1 was confined to just three districts—Bannu, Orakzai (KP), and Karachi (Sindh)—with only six cases reported. Similarly, in 2022, the 20 detected cases were limited to North Waziristan (n=17), Lakki Marwat (n=2), and South Waziristan (n=1). The situation in 2021 was even more promising, with only a single case reported in Killa Abdullah, Balochistan. This pattern indicates that in recent years, Pakistan had managed to restrict the virus to a few areas, raising hopes for complete eradication. However, the sharp increase in cases in 2024, particularly in regions that were polio-free for years, highlights the severity of the resurgence. Compounding this crisis, environmental samples testing positive for WPV1 tripled in 2024, with 628 samples from 76 districts, compared to 188 in 2023—an alarming indicator of widespread viral circulation.If these numbers weren’t concerning enough, 2025 has already witnessed two fresh cases—one from DI Khan and another from Badin, Sindh. This early onset of cases underscores that the virus is not only persisting but also spreading to new areas. If urgent action is not taken, Pakistan risks a further explosion of polio cases, undoing years of progress and threatening global eradication efforts.
Why Is Polio Making a Comeback?
Despite having one of the world’s most extensive surveillance networks and a history of rigorous vaccination campaigns, Pakistan’s polio resurgence raises pressing concerns. Experts point to several key factors behind this resurgence:
- Low Routine Immunization Coverage: Shockingly, more than half of polio cases in 2024 occurred in children who had never received a single routine vaccine. Another 14% of cases were in children over five years old, indicating a significant immunity gap. While mass immunization campaigns have been effective in reaching millions, they cannot fully replace robust routine immunization programs.
- Vaccine Hesitancy and Misinformation: Misinformation surrounding polio vaccines continues to fuel resistance, particularly in Balochistan and KP. Conspiracy theories spread through social media, distrust in health authorities, and religious misconceptions have led many parents to refuse vaccination for their children, leaving entire communities vulnerable.
- Conflict and Accessibility Challenges: Certain areas, particularly in Balochistan and KP, remain hard to reach due to insecurity, militancy, and geographical barriers. Vaccination teams often face hostility, and in some cases, life-threatening violence. Without improved access to these high-risk areas, polio will continue to thrive in these pockets of vulnerability.
- Cross-Border Transmission: Genomic sequencing of WPV1 cases in Pakistan has revealed strong links to poliovirus strains circulating in Afghanistan. The frequent movement of people between the two countries, combined with uncoordinated immunization efforts, has allowed the virus to persist and spread.
A Call to Action
Polio eradication in Pakistan requires an urgent, multi-faceted approach. Routine immunization must be prioritized alongside supplementary vaccination campaigns. Health authorities must counter vaccine hesitancy through community engagement, involving religious leaders and local influencers to combat misinformation. Insecurity issues need immediate government intervention to protect frontline workers. Furthermore, Pakistan and Afghanistan must synchronize vaccination efforts to cut off cross-border transmission routes.Pakistan has proven before that progress against polio is possible, but the current resurgence demands immediate, decisive action. Without it, the country risks not only prolonging its own polio crisis but also jeopardizing global eradication goals. The world is watching—will Pakistan rise to the challenge?
By ISID Emerging Leader, Dr. Massab Umair
Dr. Massab Umair is a Virologist and Public Health Expert specializing in disease surveillance and health systems strengthening. He is also an Emerging Leader in Infectious Diseases (ISID).
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By Aisha Abubakar,
Wednesday, February 5, 2025
Updated: Wednesday, March 5, 2025
|
The recent Ebola outbreak in Uganda has raised significant concerns regarding its potential spread, given the virus's history of rapid transmission and high mortality rates. On January 29, 2025, a 32-year-old nurse in Kampala succumbed to the Sudan strain of the Ebola virus, marking the country's first Ebola-related death in two years. This incident underscores the persistent threat of Ebola in the region and the challenges associated with containing its spread [1].
The Sudan strain of Ebola, responsible for the current outbreak, is particularly concerning due to the absence of an approved vaccine. Unlike the Zaire strain, for which vaccines exist, the Sudan strain necessitates alternative containment strategies. In response, Ugandan health authorities have initiated a clinical trial for a vaccine targeting this specific strain. Developed by the International AIDS Vaccine Initiative (IAVI), the trial is being conducted by the Makerere Lung Institute, which has received approximately 2,460 doses. The primary focus is on vaccinating contacts of confirmed cases to curb further transmission [2].
The risk of Ebola spreading in Uganda is exacerbated by several factors. Kampala, the capital city, is densely populated and serves as a major travel hub, increasing the likelihood of rapid virus transmission. The mobility of the city's 4 million residents poses significant challenges for contact tracing and containment efforts. Health officials have identified 44 contacts associated with the deceased nurse, including 30 health workers, highlighting the critical need for effective monitoring and intervention strategies [3].
Key Drivers of the Outbreak
A study by Nanyonjo et al. (2023) analyzed the drivers of Ebola transmission in Uganda’s Mubende and Kassanda districts and identified several critical causes of the outbreak [6]:
- Delays in Seeking Medical Care – Fear, stigma, and lack of awareness led many infected individuals to avoid seeking timely medical attention, allowing the virus to spread within communities.
- Traditional Burial Practices – Cultural rituals involving direct contact with the deceased significantly contributed to the transmission of the virus.
- Mistrust in Health Authorities – Some community members were skeptical of government interventions, leading to reluctance in following containment measures such as quarantine and contact tracing.
- Mobility and Trade Routes – High population movement, particularly along trade corridors, facilitated the spread of the virus beyond the initial outbreak areas.
- Healthcare Worker Exposure – Inadequate personal protective equipment (PPE) and delayed case detection led to nosocomial transmission among healthcare workers, increasing the outbreak's severity.
These findings highlight the urgent need for community engagement, improved surveillance, and culturally sensitive public health interventions to mitigate the spread of Ebola and enhance outbreak response efforts.
Conclusion
The current Ebola outbreak in Uganda underscores the critical importance of swift and coordinated public health responses. While the initiation of vaccine trials offers hope, the absence of an approved vaccine for the Sudan strain necessitates reliance on traditional containment measures, including contact tracing, community engagement, and strict adherence to infection prevention protocols.
In your opinion, how can addressing the root causes of transmission, particularly delays in seeking care, traditional burial practices, and mistrust in health authorities be mitigated to prevent the spread of this current outbreak?
By ISID Scientific Manager, Aisha Abubakar
References
- Associated Press. Uganda nurse dies of Ebola, first fatal case in two years [Internet]. 2025 [cited 2025 Feb 4]. Available from: https://apnews.com/article/762d73117fda1220f9907ad54295f1ef
- Reuters. Ebola vaccination trial launched in Uganda, WHO says [Internet]. 2025 [cited 2025 Feb 4]. Available from: https://www.reuters.com/business/healthcare-pharmaceuticals/ebola-vaccination-trial-launched-uganda-who-says-2025-02-03/
- Associated Press. Uganda health workers exposed to Ebola after nurse’s death [Internet]. 2025 [cited 2025 Feb 4]. Available from: https://apnews.com/article/fc33af48307c911c7771db825c159333
- Ssali M, et al. Transmission dynamics of the 2022 Ebola outbreak in Uganda: a mathematical modeling approach. J Infect Dis [Internet]. 2023 [cited 2025 Feb 4];228(5):678–85. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC11413514/
- Chowell G, Hengartner NW, Castillo-Chavez C, Fenimore PW, Hyman JM. The basic reproductive number of Ebola and the effects of public health measures: the cases of Congo and Uganda. J Theor Biol [Internet]. 2005 [cited 2025 Feb 4];229(1):119-26. Available from: https://arxiv.org/abs/q-bio/0503006
- Nanyonjo A, et al. Perceived drivers of Ebola outbreak in Uganda’s Mubende and Kassanda districts: insights from a qualitative study. BMJ Public Health [Internet]. 2023 [cited 2025 Feb 4];2(2):e001267. Available from: https://bmjpublichealth.bmj.com/content/2/2/e001267
- Kupferschmidt K. Uganda’s Ebola outbreak underscores need for Sudan strain vaccine. Nature [Internet]. 2022 [cited 2025 Feb 4]. Available from: https://www.nature.com/articles/d41586-022-03192-8
- Gostin LO, Hodge JG. The global response to Ebola in Uganda: legal and ethical challenges. BMJ Glob Health [Internet]. 2022 [cited 2025 Feb 4];7(12):e010982. Available from: https://gh.bmj.com/content/7/12/e010982
- Bell BP, Damon IK, Jernigan DB, Nichol ST. Overview, control strategies, and lessons learned in past Ebola outbreaks. N Engl J Med [Internet]. 2020 [cited 2025 Feb 4];382(4):393-403. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6831630/
-
Bausch DG, Towner JS, Dowell SF, Kaducu F, Lukwiya M, Nichol ST, et al. Assessment of the risk of human-to-human transmission of Ebola virus in healthcare settings. J Travel Med [Internet]. 2024 [cited 2025 Feb 4];31(5):taae079. Available from: https://academic.oup.com/jtm/article/31/5/taae079/7691187
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By ISID Emerging Leaderm Vrinda Nampoothiri,
Sunday, December 1, 2024
|
Antimicrobial Resistance (AMR) has been identified as a global health and developmental challenge. The Global Research on Antimicrobial Resistance (GRAM) project findings for 2019 estimated 4.95 million deaths due to drug-resistant bacterial infection, with a higher burden on low-resource settings (1).
The 79th United Nations General Assembly (UNGA) High-Level Meeting on AMR was held in September 2024, and global leaders committed to reducing the AMR death rate annually by 10% (2). While new drug development can be challenging, various new drugs show promising antibacterial activity. However, access to these drugs is still predominantly only in high-income countries. While it is important that Low- and middle-income countries (LMIC) also have access to these antibiotics, there is the dilemma of managing access without excess use of antibiotics (3).
Understanding the socio-economic drivers of AMR, such as gender, living conditions, access to healthcare and climate change, can help develop sustainable interventions for mitigating AMR (4). These social determinants of health intersect and interact with one another to shape an individual’s societal experiences. Such interactions can be better understood by adopting an intersectional lens. Understanding the experiences of AMR from individuals differently impacted by AMR due to these social determinants of health contributes to building culture-sensitive and responsible interventions against AMR (5).
LMICs also face challenges around access to clean water, sanitation, and health (WASH), which contributes to their high infectious disease burden. This issue is more prominent in the rural areas and marginalized populations, including women and girls, of these countries (6). Women and girls also have inadequate access to healthcare. They are more exposed to drug-resistant infections due to their role in food production, caregiving, and water collection and a higher rate of sexual violence. Women also constitute 70% of the healthcare workforce, which contributes to their exposure to drug-resistant infections (7).
In LMICs like India, the caste system poses a challenge to ensuring equitable access to healthcare. The caste system represents a hierarchy of social roles that hold inherent characteristics. The status attached to one’s caste has been passed down over the generations, changing it from a social role to a hereditary role (8). People who belong to the lower castes, such as Dalits, are limited to occupations such as domestic laborers, scavengers, and sweepers and have lower access to education and healthcare in addition to facing social discrimination in society (9). In many other parts of the world, race also affects health-seeking and health-providing behaviors. These social constructs can also influence their access to education and income levels.
The use of intersectional research in health care is gaining momentum now. Intersectional research can be conducted by using various qualitative, quantitative, and mixed methods, amongst which qualitative methods like ethnography are the most common. When conducting such studies, researchers must know how their biases, shaped by their social constructs, can influence their research work. Although it may not be possible to eliminate such biases, cultivating this self-awareness enables researchers to consciously avoid letting personal judgments distort their findings. In the Wellcome Trust funded the PROTEA study that we are currently undertaking, which investigates the intersection of socio-economic and cultural drivers on AMR and its health-seeking and health-providing behaviors, potential researcher biases will be addressed through reflexivity, methodological and analytical triangulation, and working closely with research participants and collaborators (10).
It is also important that these cultural drivers are considered in AMR policies. In a review of National Actional Plans, it was found that there is little to no recognition of addressing the cultural drivers of health-seeking and health-providing behaviors (11). It is important that AMR interventions include an intersectional approach and are contextually fit and culturally sensitive. Multisectoral collaboration is also key in tackling AMR. Healthcare professionals, researchers, community members, activists, policymakers, environmentalists, veterinarians, climate change experts should join hands to develop interventions against AMR from a One Health perspective.
By ISID Emerging Leader, Vrinda Nampoothiri
References
- Global Research on Antimicrobial Resistance. Global burden of bacterial AMR. https://www.tropicalmedicine.ox.ac.uk/gram/research/global-burden-of-bacterial antimicrobial-resistance
- World leaders commit to decisive action on antimicrobial resistance. https://www.unep.org/news-and-stories/press-release/world-leaders-commit-decisive-action-antimicrobial-resistance
- Patel TS, Sati H, Lessa FC, Patel PK, Srinivasan A, Hicks LA, et al. Defining access without excess: expanding appropriate use of antibiotics targeting multidrug-resistant organisms. The Lancet Microbe. 2024 Jan 1;5(1):e93–8.
- Anderson M, Ljungqvist G, van Kessel R, Saint V, Mossialos E. The socioeconomic drivers and impacts of Antimicrobial Resistance: Implications for policy and research. Copenhagen: European Observatory on Health Systems and Policies, WHO Regional Office for Europe; 2024
- Charani E, Mendelson M, Ashiru-Oredope D, Hutchinson E, Kaur M, McKee M, et al. Navigating sociocultural disparities in relation to infection and antibiotic resistance-the need for an intersectional approach. JAC Antimicrob Resist. 2021 Oct 1;3(4):dlab123. doi: 10.1093/jacamr/dlab123.
- Biswas S, Adhikary M, Alam A, Islam N, Roy R. Disparities in access to water, sanitation, and hygiene (WASH) services and the status of SDG-6 implementation across districts and states in India. Heliyon. 2024 Sep 30;10(18):e37646.
- WHO releases guidance on gender inequalities and antimicrobial resistance. https://www.who.int/news/item/16-09-2024-who-releases-guidance-on-gender-inequalities-and-antimicrobial-resistance
- Sankaran S, Sekerdej M, von Hecker U. The Role of Indian Caste Identity and Caste Inconsistent Norms on Status Representation. Front Psychol. 2017 Mar 31;8:487. doi: 10.3389/fpsyg.2017.00487. PMID: 28408896; PMCID: PMC5374864.
- Thapa R, Teijlingen E van, Regmi PR, Heaslip V. Caste Exclusion and Health Discrimination in South Asia: A Systematic Review. Asia-Pacific Journal of Public Health. 2021 May 24;33(8):828.
- Charani E, Dlamini S, Koch A, Singh S, Hodes R, Laxminarayan R, et al. Power Relations in Optimisation of Therapies and Equity in Access to Antibiotics (PROTEA) Study: investigating the intersection of socio-economic and cultural drivers on antimicrobial resistance (AMR) and its influence on healthcare access and health-providing behaviours in India and South Africa. Wellcome Open Res. 2024 Jul 24;9:400.
- Charani E, Mendelson M, Pallett SJC, Ahmad R, Mpundu M, Mbamalu O, et al. An analysis of existing national action plans for antimicrobial resistance-gaps and opportunities in strategies optimising antibiotic use in human populations. Lancet Glob Health. 2023 Mar;11(3):e466-e474. doi: 10.1016/S2214-109X(23)00019-0.
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By ISID Emerging Leader, Abiodun Egwuenu,
Friday, November 8, 2024
|
On the 3rd of November 2024, the One Health Day was celebrated globally. This reminds us that the intersection of health, climate, and resistance demands cohesive, global action, a goal achievable only through a shared commitment to our interconnected world.
Climate overshoot is a reality, carrying significant ecological, health, and socioeconomic consequences. While “climate change” encompasses a range of long-term shifts in temperature, weather patterns, and atmospheric conditions largely driven by human activities, “climate overshoot” refers to temporary but severe breaches of temperature limits that may prompt irreversible environmental damage.
Countries agreed to pursue efforts to limit global warming to below 1.5 - 2°C at the 2015 Paris Climate Agreement. According to the Climate Overshoot Commission, “climate overshoot” refers to crossing the 1.5 °C threshold. One of the less discussed aspects of climate overshoot is its impact on health systems, particularly with respect to antimicrobial resistance. Antimicrobial Resistance (AMR) occurs when bacteria, viruses, fungi, and parasites adapt and become resistant to medications that successfully treat these infections, is a global public health emergency. Climate change and AMR are linked through several mechanisms.
- Agricultural Pressures: Climate impacts on agriculture, such as altered rainfall patterns and drought, may drive a higher reliance on antibiotics to prevent infections in stressed animals, intensifying antibiotic use and resistance. In regions with weak regulatory oversight, this can lead to unchecked AMR spread, impacting local and global health.
- Changing Ecosystems and Disease Vectors: Rising temperatures can broaden the habitat of disease-causing organisms and their carriers, such as ticks and mosquitoes, leading to increased disease exposure. For example, warmer climates can expand the range of vector-borne diseases (such as malaria or dengue), increase respiratory illnesses due to pollution and wildfires, and lead to waterborne disease outbreaks after floods. This expansion of infectious diseases could increase antibiotic usage, consequently hastening the development of antibiotic resistance.
- Human Migration and Overcrowding: Climate overshoot may trigger human migration and displacement due to extreme weather events or sea-level rise, leading to overcrowded living conditions and increased risk of infection. A high population density often coincides with increased antimicrobial use and poor sanitation, both facilitating the spread of AMR.
It is clear that human health is intricately tied to the health of animals and the environment, and the links between climate change, AMR, and health outcomes are undeniable. Ongoing global health initiatives recognise the need for integrated solutions. The Paris Agreement focuses on reducing emissions to maintain global temperatures below critical thresholds. Although primarily aimed at climate mitigation, the agreement also supports climate adaptation strategies to help buffer health systems against the consequences of overshoot scenarios, including AMR. The WHO’s Global Action Plan on AMR highlights a One Health
approach, stressing collaboration across the human, animal, and environmental health sectors. This plan acknowledges that climatic factors play a role in the spread of AMR, particularly in agriculture and other ecosystems. The One Health High-Level Expert Panel (OHHLEP) emphasises the importance of integrated approaches in addressing AMR and climate health impacts. OHHLEP helps governments align climate and AMR strategies by advocating for the One Health approach, fostering health resilience across sectors.
The impact of climate overshoot on AMR highlights the need for unified action. It is important that we need to reinforce policies that bridge health, environment, and
Agriculture by:
- Reducing Antibiotic Pollution: Strengthening regulations regarding antibiotic use in agriculture and promoting clean water access can protect the environment from antibiotic residues, thus slowing the spread of AMR.
- Supporting Sustainable Agriculture: Climate-resilient crops and livestock practices help to reduce the need for antibiotics. Investing in climate-smart agriculture can mitigate climate impact and limit AMR.
- Investing in Climate-Resilient Health Systems: This refers to building health healthcare systems equipped to handle the increased disease burden and health challenges triggered by climate overshoot. Climate changes can lead to increased occurrence of outbreaks. There is a need to deploy improved health data monitoring systems, especially genomic epidemiology for infectious diseases, improve access to healthcare services and institute community-driven preventive strategies (vaccination, health promotion).
Climate change, health, resistant infections, and antimicrobial use are all entwined within our ecosystem. By investing in sustainable climate-smart healthcare practices, One Health policy, and eco-friendly practices in agriculture, we can truly state that we are committed to a future where the health of people, animals, and the planet is protected for generations to come.
Written by ISID Emerging Leader, Abiodun Egwuenu
References
- IPCC. (2023). Climate Change 2023: Synthesis Report Summary for Policymakers.
- World Health Organization. (2015). Global Action Plan on Antimicrobial Resistance.
- Murray, C. J., Ikuta, K. S., Sharara, F., Swetschinski, L., Aguilar, G. R., Gray, A., & Han, C. (2022). Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. The Lancet, 399(10325), 629-655.
- United Nations. (2015). Paris Agreement.
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By ISID Emerging Leader, Laura Oliveira,
Saturday, October 5, 2024
Updated: Monday, October 7, 2024
|
Meningitis is a deadly and debilitating infectious disease that can be caused by bacteria, viruses, fungi, and parasites. Meningitis affects people of all ages across the globe, but mainly young children. The disease causes an inflammation of the membranes that envelop the brain and spinal cord (meninges), and the symptoms start quickly. Although meningitis can be caused by several microbes, bacterial meningitis is the most dangerous form of the disease. Most bacterial meningitis cases are caused by four pathogens: Neisseria meningitidis (meningococcus), Haemophilus influenzae, Streptococcus pneumoniae (pneumococcus) and Streptococcus agalactiae (Group B Streptococcus, GBS). It is estimated that 1 in 6 people who get bacterial meningitis will die and 1 in 5 people who survive will have long-lasting disabilities like deafness, epilepsy, paralysis, and cognitive impairment. In 2019, bacterial meningitis accounted for 16.3 million disability-adjusted life years (DALYs) and low- and middle-income countries (LMIC) were the most affected regions (>95%). Thus, populations with low socioeconomic status are more likely to die from meningitis or suffer from its long-lasting disabilities.
Although meningitis is considered a global health problem, the highest burden of the disease is found in LMIC, especially the “meningitis belt” of sub-Saharan Africa. The meningitis belt encompasses 26 countries and is known for the high frequency of severe meningitis epidemics reported in the region. Meningitis epidemics have also been reported in other regions, including Latin America and Asia, and demand huge financial resources from the healthcare system to afford patients’ treatment, rehabilitation regimens, and other required control and prevention measures. Considering the economic and social scenario of LMIC, meningitis reinforces and amplifies the inequity that already exists in these countries and highlights the lack of access to health care systems experienced by vulnerable populations.
Safe and effective vaccines to prevent meningitis caused by N. meningitis, H. influenzae, and S. pneumoniae are available, and vaccines against GBS are in advanced development. The meningitis vaccines already available have been successful in decreasing the disease burden, as demonstrated by the eradication of epidemics by Meningococcus serogroup A in the meningitis belt and the reduction in the global meningitis burden due to the implementation of vaccines against H. influenzae type b (Hib) and pneumococcal conjugate vaccines (PCV). These vaccines confer protection not only to the vaccinated people but to the entire population (herd effect) and impact other infectious diseases caused by these pathogens, like pneumonia and sepsis. However, the vaccines against pneumococcus and meningococcus prevent the major but not all serotypes and serogroups able to cause meningitis, and they were not implemented by all LMIC – greatest gaps are observed in middle-income countries.
Additionally, the reduction rate on the meningitis burden (2000-2019 – meningitis deaths reduced by 39%) was lower than the reduction observed for other vaccine-
preventable diseases (2000-2019 – deaths due to tetanus and measles reduced by 77% and 86%, respectively).
In 2021, the World Health Organization (WHO) together with partners (governments, global health organizations, academia, private sector, among others),
launched a global roadmap to defeat meningitis as a public health threat - DEFEATING MENINGITIS BY 2030 - A GLOBAL ROAD MAP. The roadmap focuses on the four major agents of bacterial meningitis and is based on three visionary goals: to eliminate bacterial meningitis epidemics, reduce cases of vaccine-preventable bacterial meningitis by 50% and deaths by 70%, and reduce disability and improve the quality of life after meningitis due to any cause. These goals will be achieved by integrated actions organized in five pillars, which are prevention and epidemic control, diagnosis and treatment, disease surveillance, care and support, and advocacy and engagement. The global road map is already in course, and it is expected that the achievement of the visionary goals will avert 2,750,000 meningitis cases and 920 000 deaths by 2030. In addition, the global road map will have an impact on reducing the burden of other serious infectious diseases (pneumonia, sepsis), tackling antimicrobial resistance spread, and reducing health-care costs and social inequalities.
The WHO and its partners have taken the lead in the fight against meningitis, but the civil society is also an important ally in this war. It is critical to raise awareness of meningitis and its health and socioeconomic impacts among the global population. The World Meningitis Day, celebrated on October 5th, is a unique moment in the year dedicated to uniting people across the world to fight against meningitis and help save lives. This global movement started in 2009 by a community of people affected by meningitis and is supported by the Confederation of Meningitis Organisations (CoMO) and the Meningitis Research Foundation. The World Meningitis Day involves an active campaign via a dedicated website and social media to share people’s previous experience with meningitis and inform the population across the globe about how to prevent and defeat the disease. Everyone can take action in the campaign and help raise awareness of meningitis by either telling their own story, using the social media toolkit, contacting local politicians, or making a donation. The path towards a world free of meningitis is challenging, but with united action from all sectors (global health organizations, private sector, governments, civil society, academia), we can achieve this ultimate goal and make a lasting impact on global health.
Written by ISID Emerging Leader Laura Oliveira
References
Investing to defeat meningitis and beyond – World Health Organization (WHO)
Defeating meningitis by 2030: a global road map – World Health Organization (WHO)
Introducing World Meningitis Day: 5th October – Meningitis Research Foundation
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By ISID Emerging Leader, Dr. Elita Jauneikaite,
Thursday, September 12, 2024
Updated: Thursday, September 12, 2024
|
This month, a high-level meeting on antimicrobial resistance (AMR) organized by The UN General Assembly will take place on the 26th of September in New York, USA (1). Global leaders will come together and agree on actions needed to tackle the threat of AMR.
AMR is the ability of a pathogen to survive exposure to antimicrobial agents that previously were an effective treatment. Such pathogens usually acquire AMR through mutations in specific genes or through gene transfer; when a microorganism acquires multiple genetic changes making it resistant to multiple antimicrobials, this pathogen is then called a multi-drug resistant organisms (MDRO), more commonly known as a “superbug”. It has been estimated that 4.95 million deaths were associated with AMR in 2019 (2), with this number predicted to increase to 10 million per year by 2050 (3). As we all know too well, pathogens do not recognize borders and can spread between environments, which means that they are everyone’s problem, and global equitable solutions need to be sought out.
Whole genome sequencing (WGS) allows us to look at the full genetic makeup of the pathogen such as genetic features that allow us to characterize them based on genotype, virulence genes and genomic changes or acquired genes conferring resistance to antibiotics; as well as providing insights into evolutionary changes in pathogen populations when investigating genomes from longitudinal studies. Overall, genomics has great potential to assist outbreak investigation, pathogen surveillance and help to detect difficult to grow pathogens, identify novel types of pathogens and novel antimicrobial resistance determinants.
Genomics so far has been instrumental in helping to track pathogenicity of particular clinically-relevant pathogens (4), detect outbreaks and the source of the outbreak (5,6), track novel and emerging AMR trends (7,8) and understand better how AMR can spread through horizontal gene transfer in hospital settings (9,10). Additionally, genomics has put a higher importance on looking into AMR emergence and spread with ‘ONE Health’ view, with studies reporting on zoonotic exchange of bacterial pathogens and AMR genes between the environment, animals, and humans (11-13), understanding the drivers for exchange of AMR between different interfaces will allow to make informed actions for intervention.
How can we better utilise genomics and implement it as integral part of our fight against AMR?
A SECRIC Working Group on Genomics for AMR Surveillance (https://sedric.org.uk/working- groups/) has published 9 recommendations (14) on what needs to happen to help implement genomics into AMR surveillance whilst discussing current advantages and challenges faced for implementing genomics for AMR Surveillance in health laboratories, public health networks and One Health (15-19). WHO GLASS (Global Antimicrobial Resistance Surveillance system) has also published overview of benefits and limitations of implementing current WGS technologies into routine surveillance (20). A number of very successful workshops aimed at building capacity for bioinformatics and genomic sequencing for AMR surveillance workshops aimed at building capacity has taken place and were funded by Wellcome Trust (21) and Fleming Fund (22).
What can we do to help fight AMR?
You can help by getting involved and organising activities to engage your family, institution, public, policy members, and colleagues in learning more about AMR during World Antimicrobial Awareness Week (WAAW), which will take place from November 18 to 24, 2024.
References:
1. The UN Meeting on AMR: https://www.who.int/news-room/events/detail/2024/09/26/default- calendar/un-general-assembly-high-level-meeting-on-antimicrobial-resistance-2024
2. Murray et al, 2022: Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis; doi: https://doi.org/10.1016/S0140-6736(21)02724-0
3. O’Neil report May 2016: doi: https://amr- review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf
4. Heinz E, et al 2024: Longitudinal analysis within one hospital in sub-Saharan Africa over 20 years reveals repeated replacements of dominant clones of Klebsiella pneumoniae and stresses the importance to include temporal patterns for vaccine design considerations, doi: https://doi.org/10.1186/s13073-024-01342-3
5. Self JL et al, 2019: Multistate Outbreak of Listeriosis Associated with Packaged Leafy Green Salads, United States and Canada, 2015-2016, doi: https://doi.org/10.3201%2Feid2508.180761
6. Bottichio L, et al, 2020: Shiga Toxin-Producing Escherichia coli Infections Associated With Romaine Lettuce-United States, 2018, doi: https://doi.org/10.1093/cid/ciz1182
7. Alba P, et al, 2018: Molecular Epidemiology of mcr-Encoded Colistin Resistance in Enterobacteriaceae From Food-Producing Animals in Italy Revealed Through the EU
Harmonized Antimicrobial Resistance Monitoring, doi: https://doi.org/10.3389/fmicb.2018.01217
8. Forde BM, Zowawi HM, et al, 2018: Discovery of mcr-1-Mediated Colistin Resistance in a Highly Virulent Escherichia coli Lineage, doi: https://doi.org/10.1128%2FmSphere.00486-18
9. Evans DR, et al, 2020: Systematic detection of horizontal gene transfer across genera among multidrug-resistant bacteria in a single hospital, doi: https://doi.org/10.7554/eLife.53886
10. Wan Y, Myall AC, Boonyasiri A, 2024: Integrated Analysis of Patient Networks and Plasmid Genomes to Investigate a Regional, Multispecies Outbreak of Carbapenemase-Producing Enterobacterales Carrying Both blaIMP and mcr-9 Genes, doi: https://doi.org/10.1093/infdis/jiae019
11. Mwapasa T., et al, 2024: Key environmental exposure pathways to antimicrobial resistant bacteria in southern Malawi: A SaniPath approach, doi: https://doi.org/10.1016/j.scitotenv.2024.174142
12. Cocker D., et al 2023: Investigating One Health risks for human colonisation with extended spectrum β-lactamase-producing Escherichia coli and Klebsiella pneumoniae in Malawian households: a longitudinal cohort study, doi: https://doi.org/10.1016/s2666-5247(23)00062-9
13. Mourkas E., et al, 2024: Proximity to humans is associated with antimicrobial-resistant enteric pathogens in wild bird microbiomes, doi: https://doi.org/10.1016/j.cub.2024.07.059
14. Harnessing genomics for AMR surveillance Policy Brief: https://sedric.org.uk/wp- content/uploads/2022/06/SEDRIC_infographic_23-06-2022.pdf
15. Baker KS, Jauneikaite E., et al, 2023: Evidence review and recommendations for the implementation of genomics for antimicrobial resistance surveillance: reports from an international expert group; doi: https://doi.org/10.1016/s2666-5247(23)00281-1
16. Jauneikaite E. et al, 2023: Genomics for antimicrobial resistance surveillance to support infection prevention and control in health-care facilities, doi: https://doi.org/10.1016/s2666-5247(23)00282-3
17. Baker KS, et al, 2023: Genomics for public health and international surveillance of antimicrobial resistance, doi: https://doi.org/10.1016/s2666-5247(23)00283-5
18. Muloi DM, et al, 2023: Exploiting genomics for antimicrobial resistance surveillance at One Health interfaces, doi: https://doi.org/10.1016/s2666-5247(23)00284-7
19. Wheeler NE, et al, 2023: Innovations in genomic antimicrobial resistance surveillance, doi: https://doi.org/10.1016/s2666-5247(23)00285-9
20. GLASS WGS for surveillance of AMR: https://www.who.int/publications/i/item/9789240011007
21. https://coursesandconferences.wellcomeconnectingscience.org/news_item/uniting-against- antimicrobial-resistance-in-africa-a-collaborative-effort-to-build-capacity-in-genomic-surveillance-of-amr/
22. https://www.flemingfund.org/publications/going-into-battle-future-of-pathogen-genomics-and-bioinformatics-in-africa-amr/
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By Aisha Abubakar,
Friday, July 12, 2024
Updated: Friday, July 12, 2024
|
With the end of the annual Hajj pilgrimage to Mecca came reports of the resurgence of COVID-19 in some West African countries, such as Senegal and Togo. Mass gatherings have historically been linked to the spread of Infectious Diseases like COVID-19, cholera, influenza, norovirus infections, and meningitis.
Typically, mass events are attended by a sufficient number of people to strain the planning and response resources of the host community, state/province, nation, or region where it is being held.
Can mass gatherings like the Hajj be better managed to prevent outbreaks of infectious diseases like COVID-19 among returnee participants?
This post has not been tagged.
Permalink
| Comments (0)
|
|